Poor mental health worldwide has a negative impact on other global public problems. This article will explore how an improvement in mental health could impact educational outcomes, economic outcomes, prevalence of non-communicable diseases and crime rates and substance abuse.
Improvement in mental health can help decrease school dropout rates
From a macroeconomic perspective, education is a key determinant of a person’s health. Countries with higher levels of education tend to have better national health conditions. Studies also reveal post-secondary education to be an especially significant influence on life expectancy, infant mortality, child vaccination rates as well as employment rates and the economic situation.
Unfortunately, based on data provided by Organisation for Economic Co-operation and Development (OECD), 20% of students dropout of school before reaching upper secondary levels. This means that one in five students face higher risk of poverty, unemployment, morbidity and mortality rates. Improvement in mental health however, can help relieve the situation as scientific evidence indicates that an improvement in mental health condition in school can decrease dropout rates.
Using a study of 3146 Danish students based on self-reported mental health surveys, researchers found that poor mental health was significantly associated with dropout among students in vocational and higher education.
Interestingly,researchers found that male students in higher education had five times the risk of dropout when reporting poor mental health. This leads researchers to conclude that poor mental health could be a predictor of dropout in males students. Whereas for female students, despite more of them reported to have mental health difficulty (29% of female students reporting poorer mental health as opposed to 19% in males), female students are found to be more likely to complete their education.
Researchers also noted a significant underreporting among Danish male students, which could be linked to the stoic perspective that reporting poor mental health is implying weakness. Therefore, there could be an underestimation of poor mental health in males, leading to the substantially higher risk of dropout.
Despite finding stark differences between male and female students when it comes to mental health conditions and dropout rates, globally there isn’t enough gender specific mental health research for the research team to delve deeper into what may possibly cause these differences in findings. This lack of understanding also inhibits the possibility of gender specific mental health intervention and support methods.
On the other hand, researchers also found that students above elementary levels have a significantly higher risk of dropout. This calls for the increased importance of mental health support and counselling especially in secondary and tertiary school settings.
To further improve mental health conditions and dropout rates, conventional grade-based dropout prevention intervention needs to be modified to include mental health condition as another metric for interventions. To achieve this, schools need to conduct mental health surveys regularly to ensure the student’s mental health conditions are in check. There’s also a need to develop methods and interventions that are more attractive to male students due to their specific help seeking behaviours.
Improvement in mental health leads to improvement in the economy
According to Richard Layard, a labour economist at LSE, mental illness is a disease of the working age, it not only causes massive suffering but also great economic waste. Through his paper, he proposed that investment in evidence-based psychologivcal therapies should be ‘at the heart of public policy making’ due to the economic benefits it brings.
Psychological therapy boosts employment and output. If mentally ill people worked as much as the rest of the population, total employment and GDP can increase by 4% in the UK, that would mean billions more in output. The gains exceed the cost of treatment.
Improvement in population mental health also decreases welfare cost and cost for physical healthcare. This is because for each $1 spent, roughly $1 is saved on welfare benefits and another $1 is saved on physical health care. All in all, psychological treatment can reduce a person’s annual physical health care costs by 20%.
Furthermore, people with mental health problems who are also physically ill typically use 60% more physical health care than equally ill people without mental health problems. The extra physical care of people with a mental illness costs close to 1% of national income.

Progress in evidence-based psychological therapies, especially cognitive behavioural therapy, has resulted in 50% recovery rates for people with clinical depression or chronic anxiety disorders and substantial improvements for others. Therapy also halves the likelihood of a relapse.
Demonstrating that spending on mental health has economic benefits can help governments justify new investments in mental health, as in the case of the mental health strategy in England.
However,in a global context, one major reason for the low funding priority given to mental health initiatives and research is the high level of stigma associated with mental health problems and many countries struggle to counter this stigma.
Improvements in mental health could reduce the prevalence and impact of non-communicable diseases
Non-communicable diseases common to high-income countries are cardiovascular disease (CVD), diabetes, and obesity. There are clear associations between depression, PTSD, anxiety and developing CVD or experiencing worsening symptoms of CVD. Stress, isolation, and inability to stay on medication as a consequence of symptoms of these mental disorders have been suggested as some reasons for the link. Thus tackling the impact of mental disorders is likely to contribute to a reduction in the prevalence of CVD. However, there is little evidence to show that there is a single method or treatment that works to reduce both symptoms of a mental disorder/s and symptoms of CVD.
Sedentary behaviour as a consequence of the symptoms of some mental disorders put those who suffer from them at high risk for obesity and associated health conditions such as diabetes. There is evidence to show that physical activity interventions can reduce symptoms of mental disorders such as depression and lead to a more active lifestyle, in turn reducing the risk of obesity.
Importantly, there is evidence to show that those who already have CVD, diabetes or obesity are more likely to develop mental disorders such as depression. For example, a study in 2015 revealed that those with obesity may be more vulnerable to developing major depressive disorder (MDD). A reduction in the impact of non-communicable disease could in turn reduce the prevalence of mental disorders.
Non-communicable diseases have a significant impact on low and middle income countries. The number of non-communicable health conditions in low and middle income countries is on the rise. Non-communicable diseases cause nearly half of all fatalities in the age group 15-59 in almost all low and middle income countries.
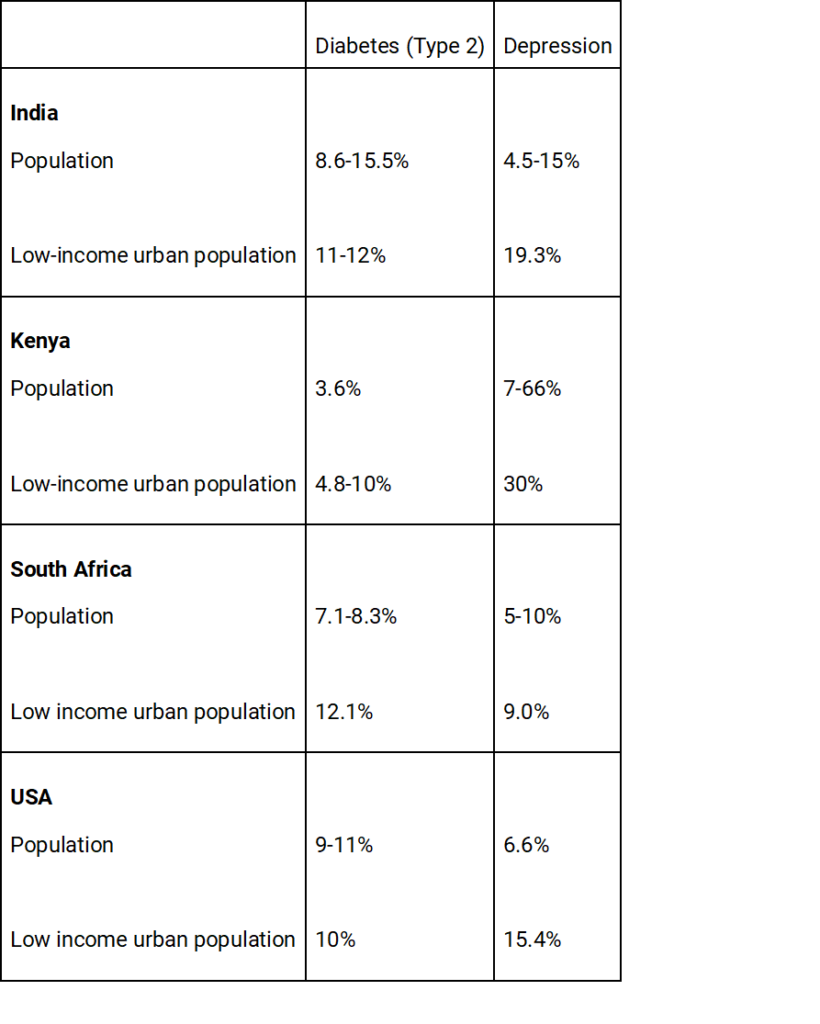
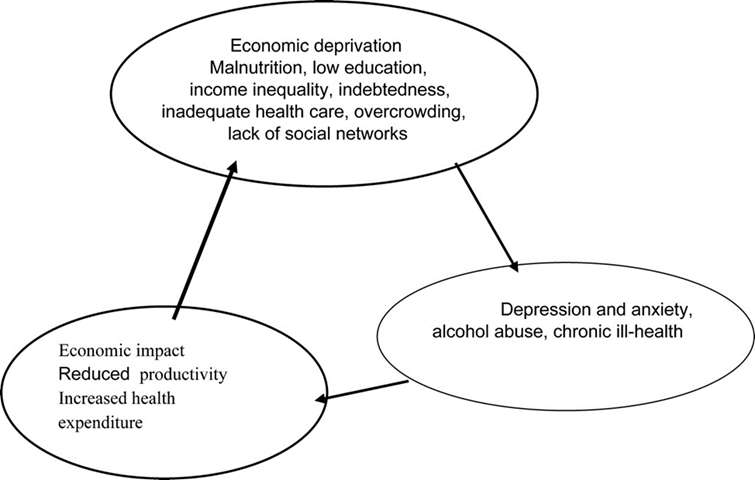
Type 2 diabetes is a common non-communicable disease in low and middle income countries. Globally, cases of depression often co-occur with cases of type 2 diabetes. Research has found that poverty significantly contributes to increased depression and diabetes cases in low and middle income countries. This is because impoverished families are often stressed by poor income or social changes such as migration. To decrease this stress, and thus cases of diabetes and depression, it is important that interventions strike at the vicious cycle of poverty.
Prevalence of Diabetes (type 2) and Depression in India, Kenya, South Africa and the USA
A syndemic approach
Many argue that a syndemic approach successfully tackles the co-occurence of depression and diabetes in low and middle income countries. A syndemic is when two conditions or diseases occur together on a national or global scale. A syndemic approach takes into account the social and economic context of the country when carrying out health practices often for two co-occurring conditions.
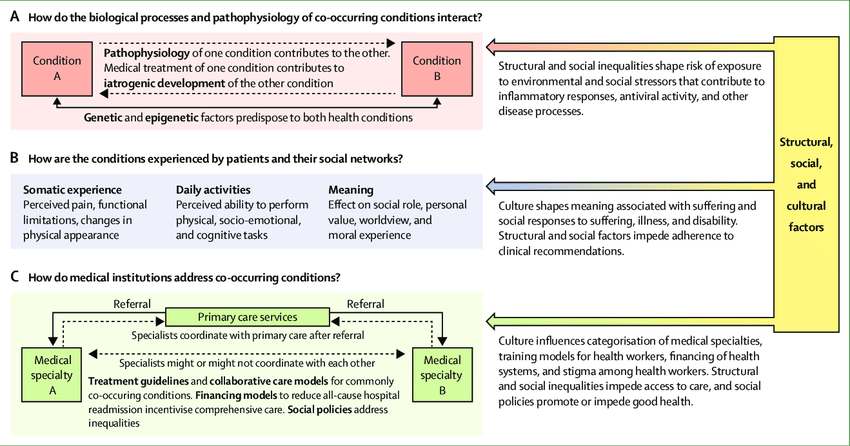
A syndemic approach may be particularly effective at tackling the co-occurence of depression and diabetes because by taking into account social and economic factors it is possible to decrease the effects of generational poverty.
From this example of depression and diabetes it is clear that mental disorders can often interact with non-communicable diseases and poverty in low and middle income countries. It is possible to surmise that to decrease the impact of certain mental disorders and non-communicable diseases the impact of poverty must be reduced.
Improvements in mental health could reduce crime rates and substance abuse
Some mental health interventions have contributed to a reduction in crime in high-income countries. For example, research in the US revealed that use of antidepressants, stimulants and psychotropic drug therapies can contribute to reducing rates of some types of crime. Moreover, greater use of mental health courts and drug courts which focus on mental health and substance abuse treatment, rather than incarceration has led to some reduction in repeat offences.
Community-based mental health interventions also have some impact. Interventions for young people and office-based mental health support have helped to reduce crime rates. A recent study showed that adding 10 more offices to a US county that provides mental health support results in a 1.6 reduction in the number of crimes per 10,000 residents.
Substance abuse in particular is treated more as a mental health rather than criminal issue in high income countries. This is because substance use disorders are often comorbid with mental disorders.
The Comorbidity Guidelines were created to help those with AOD (alcohol and other drug) and mental health conditions. They were developed in Australia in 2018. The main goal is to help individuals by considering the social and economic factors that may influence their behaviour, so that they can receive holistic treatment.
The guidelines have shown to be successful.94% of health practitioners reported having greater confidence in their practice, 89% actively use the guidelines in their practice and 59% found that their patient’s results improved due to the training provided.
Studies have shown that there is a clear link between characteristics associated with mental disorders and increased likelihood of criminal behaviour in low and middle income countries. An assessment of 39 studies found that there were associations between hyperactivity, sensation seeking, and low self-control and higher risk for anti-social behaviours such as crime. Many of the risk factors had similar effects in high income countries.
There is also a link between parental mental health issues and criminal behaviour or violence in children in low and middle income countries. It is noted that the mental health problems of parents often stem from concerns over income and poverty. Striking at the heart of the cycle of poverty in low and middle income countries could reduce the prevalence of mental health problems and thus crime.
Importantly, reducing crime rates would help reduce fear of crime. Fear of crime has shown to have some association with poor wellbeing and quality of life. Reducing crime will improve the wellbeing of those who feel vulnerable.
Given outcomes in high income countries, it is possible that improvements in mental health treatment could reduce crime rates. However, in 2007 it was found that less than <1% of the health budget in many low and middle income countries was dedicated to mental health services. 15 years on, funding for mental health is still very limited.
It is not only important that more funding is given to reduce the impact of mental health on crime, but also that mental health interventions are adjusted to be suitable for different social contexts. Risk factors for antisocial behaviour, such as hyperactivity or low-self control, can have a greater impact in societies affected by poverty. Attitudes towards delinquency also vary between countries. Mental health interventions should be adjusted accordingly.
Including mental health in the Sustainable Development Goals
In 2007, research was published in the Lancet asking for a ‘call to action’ regarding global mental health. Global mental health refers to the mental health of all populations with a particular focus on low and middle income populations. The call to action stated that there should be greater reference to mental health in the Millenium Goals. Today, mental health is part of the Sustainable Development Goals, a wider group of goals based on the aim of ‘leaving no one behind’. This change will help address the issue of poor global mental health and reduce its negative consequences.
The Movement for Global Mental Health was founded to carry out the ‘call to action’ that was stated in the 2007 publication of the Lancet. The movement held Global Mental Health Summits in 2009, 2011, 2013 and 2015.
From its start in 2007, the movement grew to have 1,304 members from 77 organisations by 2010, and continues to gain members today. The movement now includes a powerful body of researchers and other noteworthy individuals and organisations.
In a review of the movement in 2018, it was stated that they were planning to collaborate with the World Federation for Mental Health (WFMH) in the WFMH ‘Push for Mental Health’. This aims to promote visibility and rights for those with mental disorders in all countries. The review also commends the success of the organisation’s summits. Particularly, the 2009 Athens summit which had important keynote speakers including individuals who had led major HIV health campaigns.
Source: https://doi.org
What are the benefits and disadvantages of a syndemic approach to dealing with the rising number of non-communicable diseases in low and middle income countries?
Douglas-Vail (2016) explores the benefits and disadvantages of a syndemic approach through the context of HIV outbreaks. He argues that one of the benefits of the syndemic approach is that it aims to understand the interacting social and economic factors that may be at play and does not treat the disease like a stand alone entity. This enables an effective treatment of the disease. For example, it gives some insight into the global distribution of HIV. He also contends that using this approach enables practitioners to have a deep understanding of how health conditions interact such as HIV and TB.
He argues that the main limitation of the syndemic approach is the need for interdisciplinarity. It is difficult for individuals from different professions (e.g.,social work and immunology) to come together and successfully carry out the approach. There is also a lack of training programmes or guidelines on how to achieve this approach which makes collaboration even more difficult.
In 2007, research was published in the Lancet calling for greater reference to mental health in the Millennium Development Goals. Mental health is now included in the Sustainable Development Goals. What are the most important impacts of this for mental health services?
Mills (2018) explores aspects of global mental health that she hopes will improve after the inclusion of mental health into the Sustainable Development Goals. She notes that the definition of mental health varies from organisation to organisation and that the way someone defines mental health may be culturally specific. She hopes that now mental health has become a ‘global priority’ more attention will be paid to its correct definition in the future. Mills also hopes that the global burden of disease and mental health will be addressed. She points specifically to the high prevalence of comorbid substance use and mental health disorders.
Mills also explains that the economic burden of mental disorders should be lessened for those living in middle and low income countries, especially given the strong relationship between poverty and mental disorder. She also argues that mental disorders are often “a brake” on development and when treating mental disorders we should aim to eradicate social issues that contribute to their development such as poverty.
Conclusion
It is clear that improvements in mental health will have a positive impact on all the issues discussed in this article. It is key to carry out correct and effective mental health interventions to address issues such as poor educational or economic outcomes.
It is also important to integrate understanding of mental health into approaches to public issues. For example, integrating understanding of social factors including mental health into the syndemic approach to disease. Similarly, understanding of mental health is integrated into the criminal justice system through the use of mental health courts and drug courts. Finally, substance abuse and substance use disorders are effectively treated alongside comorbid mental health disorders.
A shift in the way global mental health is viewed is crucial. With the introduction of mental health into the Sustainable Development Goals, it is starting to be seen as a “global priority”. Hopefully, the improvements in mental health that come with this change will have long-term positive impacts for other public problems.
Information in the text is used from several sources (National Library of Medicine, London School of Ecnomics, The University of Chicago, University of Central Lancashire, International Scholars Journals, British Medical Bulletin, onlinelibrary, sciencedirect, iza, springer, bmcpublichealth, thelancet, frontiersin, globalmentalhealth, heinonline, comorbidityguidelines)
This article was created as part of the TeaMWork program that brings together students across the globe (University of Warwick in the United Kingdom and Monash University in Australia and Malaysia).
Authors: Angharad Wightwick, University of Warwick and Ming Yee Chan, Monash University Malaysia


